There is a lot of information out there about the risk factors for heart disease, however, a few questions consistently come up that don’t always have a straightforward answer. We will post a few articles covering several types of everyday questions about your health; today’s focus is high cholesterol and high blood pressure.
High Cholesterol
Cholesterol is the most consistent risk factor for developing CAD. There is a straight line between levels of bad cholesterol, which is called LDL cholesterol, and the development of cardiac events.
My doctor has always said my cholesterol is “fine.”
We hear this a lot, and unfortunately, many clinicians are still using older guidelines as a reference. It is tempting to look at the basic cholesterol panel done in most offices (which usually includes a total cholesterol level, a “bad” cholesterol (LDL), a “good” cholesterol level (HDL), and a triglyceride level. And if these fall in the reference range of the labs, then people are often told the test is normal. However, we don’t look at cholesterol levels in absolute any longer. The need to be put into context of your demographics and medical history to determine your 10-year cardiovascular risk. An excellent way to do this at home, if you have your most recent cholesterol readings, is the ACC Cardiovascular Risk Estimator. Plug your numbers into the calculator. If your risk of having an event in the next 10 years is greater than 7.5%, then you likely need intervention to lower cholesterol levels.
Doesn’t your body need cholesterol? Is it really safe to reduce it?
Yes, to both. Cholesterol is a combination of fats and proteins that are the essential building blocks of many or your body’s components – cell walls, hormones, and even your brain. The problem occurs when you have too much of it. And our levels tend to increase over time. So just because it was in an acceptable range 10 years ago does not mean it will still be that way today.
I eat healthy, so my cholesterol is not likely an issue.
Unfortunately, this may not be true. First, most people who believe they eat healthy, in truth, do not. It’s quite normal to not be fully aware of the common nutrition mistakes that could be hindering your health. A recent study showed that more than 60% of people who thought they had a healthy diet were not meeting daily requirements. Dietary intake of cholesterol is only one part of the story. Our body produces cholesterol as well, and if we don’t have the receptors to clear it, the levels will still rise.
High Blood pressure (Hypertension)
With a range of genetic and environmental causes, hypertension is the most common chronic disease in the United States, and its prevalence increases steadily with age.
I’m only 25, can I really have high blood pressure?
The answer is “Yes”’. While it is certainly more common as you age, high blood pressure is becoming increasingly recognized in younger people. And when it occurs, it tends to be underrecognized and undertreated. When we see elevated blood pressure in younger people, especially when it is above 140/90, we tend to consider the possibility of a secondary cause – meaning a different medical condition is causing the blood pressure to rise. Here is a list of the more common things in this category:
- Kidney disease, including narrowing of the renal arteries
- Obstructive sleep apnea, especially in those who are overweight or obese
- Endocrine conditions, with overactive glands such as thyroid (hyperthyroidism), parathyroid, and adrenal glands
- Hormone-producing tumors (such a pheochromocytoma)
- Coarctation of the aorta (congenital narrowing of the aorta after the branches to the upper extremities)
- Medications or supplements
So yes, even young people need to be on the lookout for high blood pressure. Checking every so often and maintaining regular visits with your doctor will help keep you ahead of it.
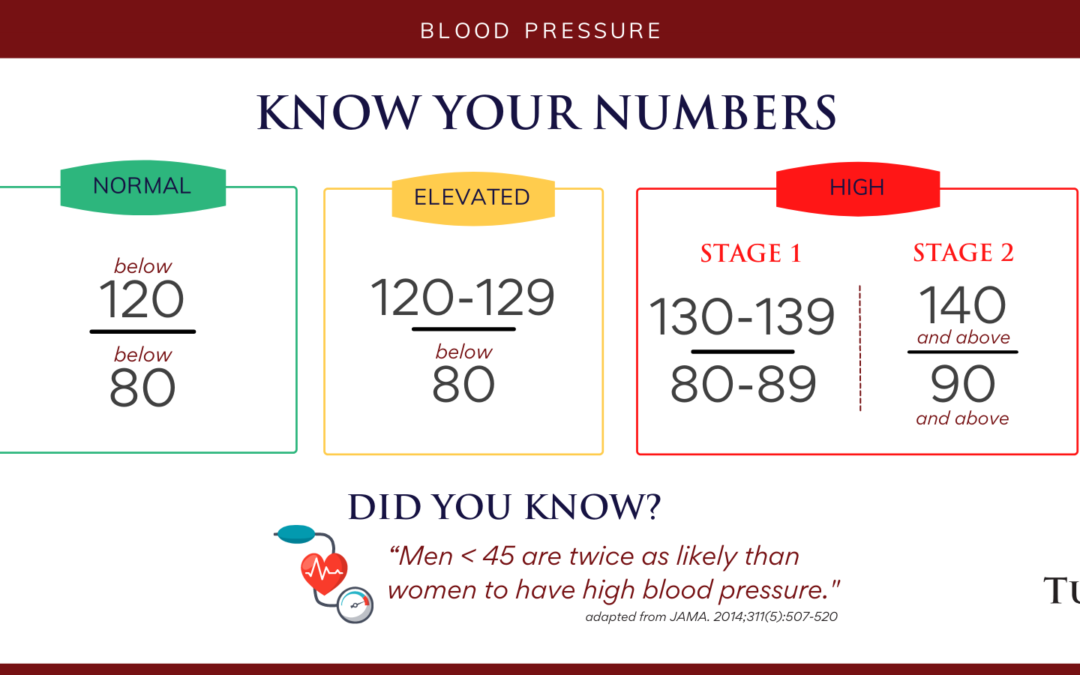
What is my blood pressure goal?
There is a lot of time spent hashing out the answer to this question. Lower is better, and the risk of complications starts to increase as soon as it climbs above 115/75. Therefore, the ideal blood pressure is less than 120/80. Once the “top number”, or systolic blood pressure gets above 120, we consider this elevated, and above 130, it is consistent with hypertension. For the diastolic (or “bottom number”), above 80 is considered in the range of hypertension. In either of these scenarios, you need a management plan which may include diet changes, activity prescription, supplementation, or medications.
- A diet high in salt
- Excessive alcohol intake – considered having more than 21 drinks per week in men
- Physical inactivity
- Elevated body weight
- Excessive use of stimulants (like caffeine)
- Over the counter medications (especially non-steroidal autoinflammatory drugs)
- Family History – twice as common if you have a family member with it
- Race – much more common and severe in certain ethnicities
My blood pressure is only high when I go to the doctor, otherwise, I feel fine. Should I be concerned?
This is a phenomenon sometimes referred to as “white coat hypertension”, a situation in which a person’s blood pressure has a consistent, significant difference between inside and outside the doctor’s office. Studies suggest this effect is quite common, occurring in the range of 10-20% of people. And it can be quite difficult to evaluate. Given the lifetime risk that comes with having high blood pressure, it is critical to ensure that the blood pressure outside the office truly is normal. Here are a few tips to consider if you blood pressure is surprisingly high in the office:
- Ensure that you are eating a diet that is low in sodium, contains the adequate nutrients, and that you are participating in regular physical activity.
- Take an honest assessment of the amount of caffeine and alcohol you are taking in as these can both have a significant effect on blood pressure levels.
- Monitor your blood pressure at home. Here is a link to a great summary on how to do it from the American Heart Association. To summarize:
- Use an automated cuff.
- Wait at least 30 minutes after a meal, and when you can rest for 5 minutes.
- Ensure you are seated in a chair with your back supported and feet on the ground.
- Aim for 2 checks per day over a seven-day period.
- Keep a log to share with your clinician.
Having high blood pressure can be sneaky because it is very unlikely to cause symptoms before the damage starts to occur. Thinking about it early, tracking it with your physician team and maintain it at your goal will keep your heart, kidney, and brain happy for years to come.
This article is not meant to be construed as medical advice, rather published for informational purposes only. Everyone’s health situation is different. As always, it is critical to discuss your symptoms, conditions, treatments, and medications with a licensed health care provider to ensure that any use is safe and effective in addressing your medical status and condition.